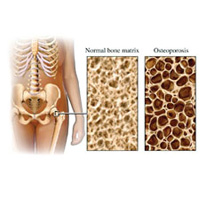
OSTEOPOROSIS
 I can still vividly picture my 80-something year old grandmother craning her neck upwards just to be able to see straight ahead while walking. She had horrible osteoporosis that left her with a stooping posture reminiscent of the Hunchback of Notre Dame. Though I felt very bad for her, I remember thinking to myself that this was just a normal part of the aging process. I wish I knew then what I know now…osteoporosis can be treated, and even prevented.
I can still vividly picture my 80-something year old grandmother craning her neck upwards just to be able to see straight ahead while walking. She had horrible osteoporosis that left her with a stooping posture reminiscent of the Hunchback of Notre Dame. Though I felt very bad for her, I remember thinking to myself that this was just a normal part of the aging process. I wish I knew then what I know now…osteoporosis can be treated, and even prevented.
WHAT IS OSTEOPOROSIS?
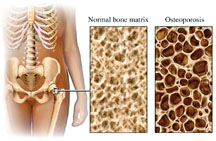
Osteoporosis is a silent disease of the bones that makes them weak and brittle, increasing the risk of fracture. Bone is living tissue that is constantly regenerating, as old bone is removed through bone resorption and replaced by new bone formation. Until the third decade of life, bone formation outweighs bone resorption, so people continue to build their bones until their mid-30’s. After that time, the balance tips in favor of bone resorption, so one cannot replace bone as quickly as it is being removed. People begin to lose bone strength as bones become thinner and structurally weaker.
Until you actually sustain a fracture or have noticeably stooped posture, the disease has no symptoms, hence, the term “silent.” A minimal impact fall that may just bruise the average person can cause significant morbidity in the osteoporotic patient in the form of traumatic or fragility fractures. The most common fractures occur at the spine, wrist and hip. Spine and hip fractures in particular may lead to chronic pain, long-term disability and even death.
WHO DOES OSTEOPOROSIS AFFECT?
Osteoporosis is a common bone disease that affects both men and women, usually as they grow older. In the United States, about 8 million women and 2 million men have osteoporosis. The greatest risk of developing osteoporosis and having a related fracture is in people over the age of fifty. In this age group, 50% of women and 17% of men will suffer an osteoporosis-related fracture at some point in their life. Caucasians and Asians are most likely to experience osteoporosis and osteoporosis-related fractures. Hispanics and African Americans also can develop osteoporosis and related fractures, but have a lower risk when compared to Caucasians and Asians. P.G. Reddy of Henry Ford Hospital, Detroit, Michigan and colleagues from Indraprastha Apollo Hospital, New Delhi, India conducted a survey of women of Indian ancestry living in the United States and found that their bone density was lower than for white women.
WHAT ARE THE RISK FACTORS FOR OSTEOPOROSIS?
There are many things that contribute to a person’s risk of developing osteoporosis. Some of these factors can be changed and other cannot. By recognizing your own risk factors, you can take measures to prevent and/or treat this condition before it becomes worse. Major risk factors include:
– Older age (especially after 50 years of age)
– Caucasian and Asian ethnic background
– Small bone structure (small body frame)
– Family history of osteoporosis or osteoporosis-related fracture in a parent or sibling
– Sex hormone deficiency, particularly estrogen deficiency, both in women (e.g. menopause – surgical or natural) and men
– Anorexia nervosa
– Cigarette smoking
– Alcohol abuse
– Low dietary intake or absorption of calcium and vitamin D
– Sedentary lifestyle or immobility
– Previous history of fracture after minimal trauma
– Medications: corticosteroid medications such as prednisone; excess thyroid hormone replacement (Synthroid, Levoxyl); the blood thinner heparin; certain anti-convulsant medications such as phenytoin (Dilantin), etc.
– Certain diseases such as endocrine disorders (hyperthyroidism, hyperparathyroidism, Cushing’s disease, etc.), inflammatory arthritides (rheumatoid arthritis, ankylosing spondylitis, etc.), kidney failure, and intestinal disorders that affect absorption of nutrients (celiac disease, ulcerative colitis, etc.)
HOW IS OSTEOPOROSIS DIAGNOSED?
A specialized type of x-ray called the dual energy x-ray absorptiometry (DEXA) is the best current test to measure bone mineral density (BMD). The test is quick and painless, and is similar to having an x-ray taken, but uses much less radiation. Usually the BMD is checked at the spine and one or both hips, but occasionally the wrist or heel may be measured.
The results of the DEXA test compared to the BMD of young, healthy individuals, resulting in a measurement called a T-score. If your T-score is –2.5 or lower, you are considered to have osteoporosis and therefore at high risk for a fracture. T-scores between –1.0 and –2.5 are generally considered to show osteopenia, the precursor to osteoporosis. The risk of fractures generally is lower in people with osteopenia when compared with those with osteoporosis but, if bone loss continues, the risk for fracture increases. However, a person with a T-score falling within the osteopenia range who sustains a fragility fracture is defined as having osteoporosis.The DEXA scan is usually repeated every 2 years to monitor any changes in BMD and also to monitor the effects of treatment.
 HOW CAN ONE PREVENT OSTEOPOROSIS FROM DEVELOPING OR WORSENING?
HOW CAN ONE PREVENT OSTEOPOROSIS FROM DEVELOPING OR WORSENING?
– Make sure there is adequate calcium in your diet (see table); and remember, it’s never too early to start counting calcium mg in your diet – I recommend to my young adult patients to monitor their calcium intake NOW – there’s no need to wait until you’re 50. If pregnant or lactating – Get adequate vitamin D intake, which is important for calcium absorption and to maintain muscle strength (400IU per day until age 60, 600-800 IU per day after age 60). Exposure to UV sunlight is also an important source of vitamin D synthesis in the skin. I would recommend no more than 10-15 minutes of sun exposure without a sunscreen twice a week. Anything more than that may increase your risk of skin cancer. Your doctor can check your blood levels of vitamin D to ensure appropriate dosage.
– Get regular exercise, especially weight bearing exercise. The tugging action of contracting muscles on bones stimulates bone formation. Exercise also improves once balance and stability, reducing one’s risk of falling and sustaining a traumatic fracture.
– For better posture in patients who already have osteoporosis, I usually prescribe a course of physical therapy with a focus on fall prevention, and back and abdominal muscle retraining.
– Other lifestyle changes such as smoking cessation and avoiding excessive alcohol will also help.
– Treating underlying conditions such as hyperthyroidism and celiac disease adequately can slow progression of osteoporosis.
HOW IS OSTEOPOROSIS TREATED?
If you are diagnosed with osteoporosis or osteopenia, your doctor may prescribe one or more of the following medications in addition to the above-mentioned dietary and lifestyle modifications. These medications are not all equal in their effectiveness in treating osteoporosis.
– Calcitonin (Calcimar, Miacalcin): This medication, a hormone made from the thyroid gland, is given usually as a nasal spray or as an injection under the skin. It has been FDA-approved for the management of postmenopausal osteoporosis and helps prevent vertebral (spine) fractures. It also is helpful in controlling pain after an osteoporotic vertebral fracture. This is the weakest of the osteoporosis treatments.
– Estrogen or Hormone Replacement Therapy (HRT): Estrogen therapy alone or in combination with another hormone, progestin, has been shown to decrease the risk of osteoporosis and osteoporotic fractures in women. However, the combination of estrogen with a progestin has been shown to increase the risk for breast cancer, strokes, heart attacks and blood clots. Although HRT is moderately effective in treating and preventing osteoporosis, its other risks add complexity of this decision. Consult with your doctor if HRT is appropriate for you.
– Selective Estrogen Receptor Modulators (SERMs): These medications mimic estrogen’s good effects on bones without some of the serious side effects such as breast cancer. Raloxifene (Evista) decreases spine fractures in women, and is approved for use only in women at this time. Like, HRT SERMs are moderately effective against osteoporosis without many of the risks of HRT like breast and endometrial cancer.
– Bisphosphonates: Alendronate (Fosamax), risedronate (Actonel) and ibandronate (Boniva) help slow down bone loss and have been shown to decrease the risk of fractures. All are pills that must be taken on an empty stomach with water. Because they have the potential for irritating the esophagus, remaining upright for at least an hour after taking these medications is recommended. Alendronate and risedronate can be taken once a week, while ibandronate can be taken once a month. An IV form of ibandronate, given through the vein every 3 months, also has been FDA-approved for osteoporosis management. There have been reports of jaw osteonecrosis (permanent bone damage of the bones of the jaw) resulting from high dose IV bisphosphonates used primarily in the management of people with underlying cancers. The risk for this problem in those taking these medications at doses recommended for osteoporosis management is not clearly established, but appears to be low. Women that are pregnant or lactating should not use Bisphosphonates.
– Teriparatide (Forteo): Teriparatide is the newest and most effective drug in our armamentum against osteoporosis. It is a form of parathyroid hormone that helps stimulate bone formation. It is approved for use in postmenopausal women and men at high risk for osteoporotic fracture. It is given as a daily injection under the skin and can be used for up to 2 years. Because of the expense of this injectable medication, most insurance companies require preauthorization for its use. Most physicians reserve this medication for patients with severe osteoporosis. If you have ever had radiation treatment or your parathyroid hormone levels are already too high, you may not be able to take this medication.
 HOW CAN ONE PREVENT FRACTURES?
HOW CAN ONE PREVENT FRACTURES?
The most worrisome consequence of osteoporosis is a fracture. Spine and hip fractures especially may lead to chronic pain, long-term disability and even death. Compression fractures of the vertebral bodies over time can lead to stooped posture. The major goal of treating osteoporosis is to prevent fractures. One must “fall-proof” one’s living environment (remove loose wires or throw rugs, install grab bars in the bathroom and non-skid mats near sinks and in the tub, etc.) Be careful when you are carrying or lifting items, as this could cause a spine fracture. Use a cane or walker if you have balance problems or other difficulties walking.
YOUR DOCTOR’S ROLE
As specialists in musculoskeletal diseases, rheumatologists can help to determine the cause of osteoporosis. They can provide and monitor the best treatments for this condition. Other doctors that frequently diagnose and treat osteoporosis are gynecologists, endocrinologists, internists, and family practitioners. Talk to your doctor today about getting tested for osteoporosis.
Adapted from the American College of Rheumatology patient education pamphlet on osteoporosis. All information above is for educational purposes only. Please consult your physician before making any treatment decisions.